Who may be offered an amniocentesis?
- Women who have had a high risk screening test result; suggesting that the fetus has an increased risk of a chromosomal abnormality.
- Women who are over the age of 37 years (some other states and countries suggest 35 years) at the estimated date of delivery.
- Women who already have had a child with a chromosomal abnormality such as Down syndrome.
- Families in which there are other inherited genetic diseases.
- Occasionally, amniocentesis is performed for other reasons, particularly if an abnormality is found at the second trimester ultrasound.
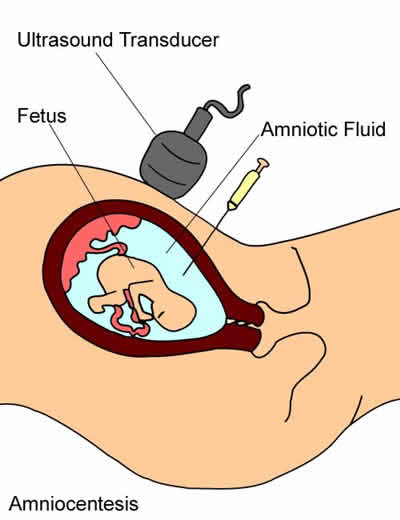
What is amniocentesis?
Amniocentesis is a test performed to assess the chromosomes of the fetus. It involves performing an ultrasound and then using the ultrasound to guide a needle through the mother’s abdomen. A small amount of the amniotic fluid which surrounds the baby is withdrawn. This is sent to a specialised genetic testing laboratory. Fetal cells within the fluid are grown in an incubator until there are sufficient cells to analyse (this takes approximately 10 days).
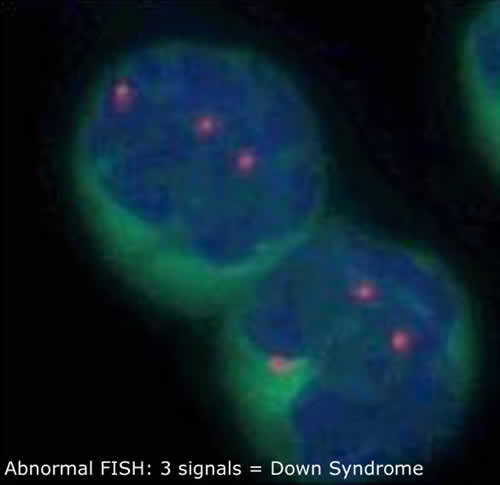
When there are sufficient cells to analyse the laboratory will issue a result, referred to as a molecular karyotype (microarray). It is possible to obtain a partial result within 24 to 48 hours. This is referred to as a FISH test. The laboratory charges an extra cost for this FISH test.
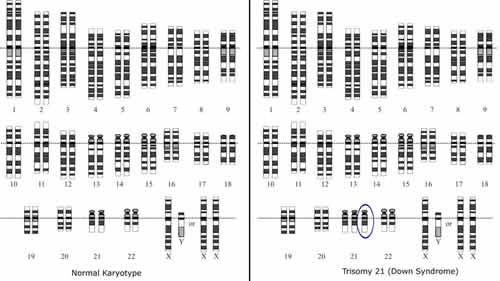
Picture of a normal karyotype (left) and Down syndrome karyotype (right)
What is the FISH Test?
FISH stands for Fluorescence In Situ Hybridisation. This is a special test which can be performed on uncultured amniocentesis or CVS samples. The result is usually available with 24-48 hours. The test does not detect all chromosomal abnormalities; this FISH test specifically looks at chromosomes 21, 18, 13, X and Y. This enables the FISH test to detect most of the common chromosomal abnormalities, particularly Down syndrome. The FISH test is also able to determine the sex of the baby.
Unfortunately this test does not attract a Medicare rebate and the laboratory will issue an extra charge for performing this test.
What is the microarray?
A molecular karyotype or microarray is a test that looks for small changes in the chromosomes that may affect health and/or normal development. These small changes are known as copy number variants (CNVs). A CNV is a small piece of extra or missing DNA and these changes may cause health issues.
Occasionally due to the indication for testing or the outcome of the microarray, further testing or investigations beyond microarray may be recommended by your Doctor or Genetic Counsellor.
How do I get my results?
When the results are ready, the laboratory will send these results directly to your genetic counsellor and/or doctor, who would usually communicate them to you. It is possible to definitively determine the sex of your baby from these results.
Is there any special preparation?
Usually there is no special preparation needed for the Amniocentesis. You can eat and drink as usual before the procedure. We recommend wearing comfortable non-restrictive clothing which allows for easy access to your abdomen.
You will need to bring a referral, a copy of your blood group report as well as any relevant test results or ultrasound reports (if these were performed elsewhere).
What to expect on the day?
An ultrasound is performed before the procedure to ensure that it is appropriate and possible to perform the Amniocentesis. The size of the fetus will be measured. The position of the placenta is then mapped and the amount of amniotic fluid assessed. Some fetal abnormalities may be visible at this stage.
The amniocentesis is then performed in the ultrasound room, this test usually only takes one to two minutes to perform. Local anaesthetic is usually not given as the thickness of the amniocentesis needle is very similar to the needles used to take blood test samples (it is the thickness of a needle not its length, which accounts for the degree of discomfort). Most people say that an amniocentesis is not much more uncomfortable than having a blood test from your arm.
If you have a Rhesus negative (Rh-ve) blood group then anti-D would be issued after the procedure.
What should I do after the procedure?
Although you are able to drive yourself home after the test most people appreciate having somebody with them to drive them home. Some patients will experience discomfort where the needle was inserted; Panadol®, Panadeine® (or other paracetamol based analgesia) or a warm pack may provide symptomatic relief. Aspirin based or non-steroidal analgesics are not advised (for example: naprosyn®; ponstan®). It is recommended that you take things quietly for the next two days. You may request a medical certificate, if necessary. After this you may return to normal duties.
Are there any complications from having an amniocentesis?
The risk of causing a miscarriage from an amniocentesis is quite low, no worse than 1 in 1000.
The risk of miscarriage has been shown to be directly related to the skill of the operator and the number of procedures the operator has performed. Dr Bethune has had extensive experience in both amniocentesis and chorionic villous sampling and was trained by one of the pioneers of invasive fetal procedures; associate Professor Lachlan deCrespigny.
Dr Bethune performs a large number of these procedures each year and is involved in teaching these procedures to obstetricians who choose to further specialize in the field of prenatal diagnosis through his commitments at the Mercy Hospital for Women.
About 0.5% of patients will have some leakage of amniotic fluid through the vagina within the first 24 to 48 hours after the amniocentesis procedure is performed. 80 to 90% of these cases will resolve without any ongoing complication for the pregnancy.
Although extremely rare, it is theoretically possible that the amniotic fluid does not grow properly in the laboratory and that the laboratory is unable to obtain a result. In these cases, a second amniocentesis would be offered.

